Covid Coverage for Employees: Keeping Calm and Covered On
Why COVID-19 Changed Employee Benefits Forever

Before 2020, employee benefits was relatively stable. But when the pandemic transformed workplaces almost overnight, Covid coverage for employees became the most critical concern for millions. The crisis created a perfect storm of public health emergencies, widespread job losses, and a cascade of new, often confusing, federal and state regulations. In this new landscape, both employees and employers urgently needed clear guidance to protect their health and financial security.
Quick Answer: COVID-19 Employee Coverage Essentials
- Health Insurance Options for the Unemployed: For those who lost jobs or hours, a safety net of options became available, including COBRA continuation coverage (often with subsidies), ACA Marketplace plans with expanded financial aid, and broader eligibility for Medicaid and CHIP.
- Federally Mandated Paid Leave: The Families First Coronavirus Response Act (FFCRA) was a landmark law that provided up to 80 hours of paid sick leave and up to 10 weeks of paid family leave for specific COVID-related reasons.
- Workers' Compensation Expansions: Recognizing the risk to frontline workers, 28 states and Puerto Rico enacted measures, many creating a "presumption" that a COVID-19 infection was work-related for eligible employees.
- New Standards for Workplace Safety: Employers were tasked with implementing new safety protocols for testing, providing Personal Protective Equipment (PPE), and managing infection control based on OSHA and CDC guidance.
- Unprecedented Benefit Flexibility: Federal relief acts introduced significant changes, including COBRA subsidies, more lenient rules for accessing retirement funds, and the expansion of telehealth services.
The pandemic didn't just change how we work - it completely reshaped the landscape of employee benefits, shifting priorities and accelerating trends that will have a lasting impact. New federal laws created paid leave requirements, expanded health coverage, and offered substantial tax credits to help employers retain their workforce. Workplace safety evolved into a shared responsibility, with protocols once considered extreme becoming standard practice.
The changes were swift and often confusing, leaving many to wonder about their rights and options. I'm Kelsey Mackley from Kelmeg & Associates, Inc. My team and I have been on the front lines, helping countless individuals and businesses steer the complex world of
Covid coverage for employees. In this comprehensive guide, we will break down everything you need to know, from health insurance options after a job loss to new workplace safety standards, ensuring you are fully informed and protected.
Navigating Health Coverage After a COVID-19 Related Job Change
When the COVID-19 pandemic triggered widespread economic disruption, millions of Americans lost their jobs or had their hours reduced, putting their employer-sponsored health insurance in jeopardy. Recognizing this crisis, federal relief efforts focused heavily on ensuring continuous
Covid coverage for employees and their families. A key provision was the reinforcement of the Special Enrollment Period. Losing your job, having your hours cut, or experiencing a significant drop in income are all considered qualifying life events. These events trigger a 60-day Special Enrollment Period, allowing you to enroll in new health coverage through the ACA Marketplace outside the standard annual open enrollment window.
COBRA Continuation Coverage
COBRA has long been the default option for employees wanting to keep their exact same health plan after leaving a job. However, it comes at a steep price, as the individual becomes responsible for paying 100% of the premium plus a 2% administrative fee. The American Rescue Plan Act (ARPA) provided massive relief by creating a 100% COBRA premium subsidy for eligible individuals. This subsidy covered the full cost of COBRA premiums from April 1, 2021, through September 30, 2021. This meant six months of completely free health coverage for many families, allowing them to maintain continuity of care with their established doctors and health plan benefits during a critical period of uncertainty.
Furthermore, the government's "Outbreak Period" relief, which was made retroactive to March 1, 2020, provided crucial deadline extensions. Normally, an individual has 60 days to elect COBRA. The Outbreak Period paused this clock, giving people significantly more time to make decisions and payments without risking a lapse in coverage. For more details on these extensions, see this resource: One-Year Expiration of Outbreak Period.
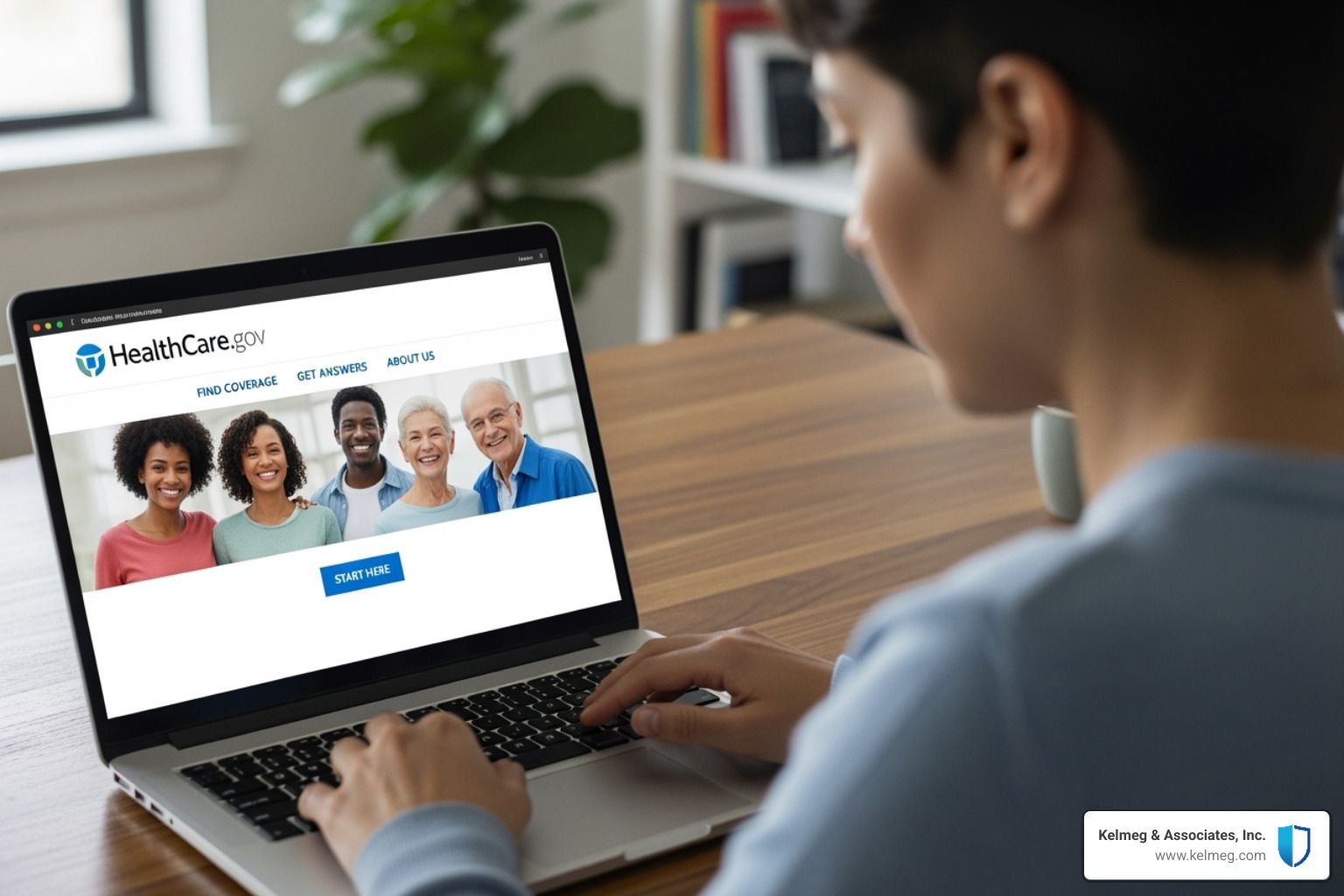
Marketplace (ACA) Health Plans
Even with temporary COBRA subsidies, many individuals found more affordable and suitable long-term coverage through the Health Insurance Marketplace, accessible via
HealthCare.gov or state-based exchanges. A COVID-related job loss automatically qualified individuals for a Special Enrollment Period to shop for these plans.
The Marketplace became an especially attractive option because the American Rescue Plan Act also significantly expanded financial assistance. It eliminated the subsidy cliff, making premium tax credits available to more people, and increased the credit amounts for those already eligible. This meant that many individuals could find high-quality plans for very low monthly premiums, sometimes even $0. A drop in income could make you newly eligible for these premium tax credits, which are designed to cap your health insurance costs as a percentage of your income. Even if you kept your job but your employer reduced their contribution to your health plan, you could still potentially access these subsidized plans. At Kelmeg & Associates, Inc., we specialize in helping Coloradans find the best marketplace options. For more information, visit: More info about ACA plans.
Medicaid and CHIP
For individuals and families with the lowest incomes,
Medicaid and the Children's Health Insurance Program (CHIP) served as an essential safety net. The economic fallout of the pandemic made millions of people newly eligible for these comprehensive, low-cost or free health programs. A key advantage of Medicaid and CHIP is that
enrollment is open year-round; you can apply at any time your financial circumstances change. Eligibility is primarily based on your Modified Adjusted Gross Income (MAGI) and varies by state. During the public health emergency, a continuous enrollment provision was enacted, preventing states from disenrolling participants and ensuring stable coverage for the nation's most vulnerable populations. It was always worth checking your state's specific eligibility requirements if you experienced a drop in income.
Employer Support: Tax Credits and Paid Leave for COVID-19
To prevent economic collapse and help businesses protect their teams, the federal government introduced several powerful financial assistance programs. These initiatives, established under the FFCRA, CARES Act, and ARPA, provided a lifeline of critical relief that helped employers maintain their workforce, cover payroll, and continue providing essential
Covid coverage for employees.
The Families First Coronavirus Response Act (FFCRA)
Enacted in March 2020, the FFCRA was a groundbreaking law that mandated employers with fewer than 500 employees to provide paid leave for specific COVID-19 related reasons. To make this feasible for businesses, the government fully reimbursed them for the cost of this leave through refundable payroll tax credits.

- Paid Sick Leave: Provided up to 80 hours of leave for reasons such as an employee being subject to a quarantine order, advised by a health provider to self-quarantine, or experiencing symptoms and seeking a diagnosis. Employees could receive up to $511 per day ($5,110 total) for their own care, or up to $200 per day ($2,000 total) if caring for someone else.
- Paid Family Leave: Offered up to ten additional weeks of leave, paid at two-thirds of the employee's regular pay. This was primarily for parents needing to care for a child whose school or place of care was closed due to the pandemic. The benefit was capped at $200 daily and $10,000 in total.
While the mandatory leave requirement expired on December 31, 2020, employers could voluntarily continue to offer this leave and claim the associated tax credits through September 30, 2021. The Department of Labor provides more details here: FFCRA Questions and Answers.
Employee Retention Credit (ERC)
The ERC, created by the CARES Act, was a refundable tax credit designed to incentivize businesses to keep employees on their payroll. Initially, the credit was for
50% of qualified wages up to $10,000 per employee for all of 2020. However, subsequent legislation, including the American Rescue Plan Act, dramatically expanded the ERC, making it much more valuable. For 2021, the credit was increased to
70% of qualified wages up to $10,000 per employee per quarter. Importantly, qualified wages included the costs of maintaining the employee's health plan, making the ERC a powerful tool for sustaining benefits. The rules were also changed to allow businesses that received a PPP loan to also claim the ERC, which was not permitted initially.
Paycheck Protection Program (PPP)
The PPP was one of the cornerstones of federal relief, providing forgivable loans to small and mid-sized businesses. These loans were designed to cover up to eight weeks of payroll costs, health benefits, retirement contributions, rent, and utilities. The most powerful feature of the PPP was its forgiveness provision. If a business used at least 60% of the loan funds for payroll costs, the entire loan could be forgiven, essentially converting it into a tax-free grant. This program was instrumental in helping millions of businesses keep their doors open and continue offering health insurance and other vital benefits to their employees. More information is available on the
Paycheck Protection Program website.
Is COVID-19 a Workplace Injury? Understanding Workers' Compensation
One of the most complex legal and insurance questions to arise from the pandemic was whether contracting COVID-19 could be considered a workplace injury. This became a critical component of Covid coverage for employees, particularly for the millions of essential workers who could not work from home. The core issue was the difficulty of proving causation for a highly contagious, community-spread virus, which challenged the very foundation of the traditional workers' compensation system.
The Challenge of Proving Workplace Contraction
Typically, common illnesses like the cold or flu are not covered by workers' compensation because it is nearly impossible for an employee to prove they contracted the illness specifically because of their job duties, rather than at the grocery store or at home. The burden of proof rests entirely on the employee. However, the unprecedented nature of the pandemic led many to argue that this standard was unfair for those whose jobs put them at a significantly higher risk of exposure. This led states to look at existing "presumptive coverage" policies, which were already in place for some first responders and assume certain occupational diseases (like respiratory illnesses for firefighters) are job-related. This concept became the primary model for handling COVID-19 claims. The
National Council on Compensation Insurance analysis offers more insight into these policies.
State-Level Changes and Presumptive Coverage
To protect essential workers,
28 states and Puerto Rico took legislative or regulatory action to make it easier for employees to file for workers' compensation for COVID-19. Eleven of these states enacted "rebuttable presumption" laws. This legal standard shifted the burden of proof: if a covered employee contracted COVID-19, the illness was presumed to be work-related. The burden then fell to the employer or their insurance carrier to present evidence proving that the infection was contracted outside of the workplace.
These presumptions were generally limited to high-risk occupations, including
first responders, healthcare staff, correctional officers, and other essential workers. The scope of coverage, the definition of an essential worker, and the duration of the presumption varied significantly by state.

| State | Worker Categories Covered | Type of Action |
|---|---|---|
| California | All workers (under specific conditions) | Legislation |
| Illinois | All essential workers | Legislation |
| New Jersey | All essential workers | Legislation |
| Utah | First responders, healthcare | Legislation |
| Vermont | All essential workers | Legislation |
| Washington | Healthcare workers, first responders (quarantined) | Executive Order/Policy |
| Wisconsin | First responders, healthcare | Legislation |
| Wyoming | All workers (under specific conditions) | Legislation |
It is important to note that many of these policies were temporary and tied to state emergency declarations, expiring as the public health crisis subsided. In Colorado, the rules have their own specifics. We help clients steer these complex regulations. For state-specific details, see our resource: More info on Covid Coverage in Colorado.
Employer Responsibilities for Workplace Safety and Covid Coverage for Employees
During the pandemic, ensuring a safe work environment became a paramount employer responsibility. Workplace safety rules changed dramatically and rapidly, requiring businesses to learn and implement new protocols based on guidance from the Occupational Safety and Health Administration (OSHA) and the Centers for Disease Control and Prevention (CDC). This effort to create a safe workplace was a fundamental part of providing Covid coverage for employees. At Kelmeg & Associates, Inc., we guide businesses through these complex responsibilities. For more on this topic, visit our page: More info on Employer Group Benefits.
Implementing Essential Safety Measures
Creating a safe workplace required a layered, multi-faceted approach to mitigate the risk of viral transmission. Key measures included:
- Ventilation: Improving indoor air quality by upgrading HVAC systems with higher-rated filters (such as MERV-13 or better), using portable HEPA filtration units, and increasing the circulation of outdoor air by opening windows and doors.
- Physical Distancing: Reconfiguring office layouts, installing physical barriers like plexiglass shields in high-traffic areas, staggering employee shifts, and using floor markers to maintain at least six feet of distance between individuals.
- Cleaning and Disinfection: Establishing and following a schedule for frequent cleaning of high-touch surfaces like doorknobs, light switches, and shared equipment, using disinfectants from the EPA's List N, which are approved for use against SARS-CoV-2.
- Exposure Notification: Developing a clear protocol for notifying employees of a potential workplace exposure while maintaining the confidentiality of the infected individual's identity, as required by the Americans with Disabilities Act (ADA).

Guidance on Testing, PPE, and Covid coverage for employees
Employers also became responsible for new screening and equipment protocols.
- Testing: While symptom and temperature screenings became common, mandatory viral testing was considered a medical examination under the ADA. Therefore, it was only permissible if an employer could show it was job-related and consistent with "business necessity". The CDC's testing information provided key guidance on strategies.
- Face Coverings: Employers were required to provide and often mandate appropriate face coverings. They also had to educate employees on the differences: cloth face coverings primarily prevent the wearer from spreading their own respiratory droplets, while surgical masks offer some protection from larger droplets. N95 respirators, when properly fitted, provide the highest level of filtration and protection for the wearer.
- Reporting: Employers were reminded of their obligation to report work-related COVID-19 fatalities to OSHA within 8 hours and in-patient hospitalizations within 24 hours.
Navigating Vaccination Policies and Covid coverage for employees
With the arrival of effective vaccines, employers faced a new set of complex policy decisions. Generally, federal law permitted employers to mandate vaccination for employees, but this right was not absolute and came with critical exceptions.
- Reasonable Accommodations: Under the ADA and Title VII of the Civil Rights Act, employers had to engage in an interactive process to provide reasonable accommodations for employees who could not be vaccinated due to a disability or a sincerely held religious belief, unless doing so would cause an undue hardship. Accommodations could include remote work, reassignment to a different position, or requiring regular testing and mask-wearing.
- Non-Discrimination: The EEOC clarified that vaccination policies could not be implemented in a way that discriminated based on age, pregnancy, national origin, or other protected characteristics. The EEOC's COVID-19 Q&A became an essential resource for employers.
- Retaliation Protection: It is illegal for an employer to retaliate against an employee for raising safety concerns, reporting an illness, or requesting a reasonable accommodation.
How COVID-19 Legislation Reshaped Employee Benefits
The CARES Act and the American Rescue Plan Act (ARPA) were monumental pieces of legislation that went far beyond creating new programs. They fundamentally altered the existing rules governing
Covid coverage for employees, introducing unprecedented flexibility for retirement savings, health plans, and administrative deadlines.
Changes to Retirement Plans (401(k)s, Pensions)
The CARES Act recognized the immense financial strain placed on families and provided significant relief for retirement plan participants:
- Coronavirus-Related Distributions (CRDs): This provision allowed eligible individuals to withdraw up to $100,000 from their retirement accounts (like 401(k)s and IRAs) without incurring the standard 10% early withdrawal penalty. To be eligible, an individual had to have been diagnosed with COVID-19 or experienced adverse financial consequences due to the pandemic. Taxes on the withdrawal could be spread out over three years, and individuals had the option to repay the distribution back into their retirement account.
- Increased Loan Limits: For a limited time, the maximum loan amount an individual could take from their retirement plan was doubled from $50,000 to $100,000.
- Suspended RMDs: Required Minimum Distributions (RMDs) for retirees were suspended for 2020. This allowed seniors to avoid being forced to sell investments in a down market to meet their RMD obligations.
These changes provided a critical financial lifeline, giving people access to their own funds during a severe economic crisis. The IRS provided detailed information on this relief:
IRS guidance on retirement plan relief.
Health and Welfare Plan Modifications
Health and welfare benefits also saw significant modifications, many of which have become permanent fixtures of the benefits landscape:
- COVID-19 Testing and Services: Most health plans were required to cover COVID-19 testing, and later vaccines, at no cost to the member, eliminating financial barriers to care.
- Telehealth Expansion: The pandemic boostd the adoption of telehealth. Regulations were relaxed to allow virtual doctor visits to be covered on par with in-person visits and to permit the use of common platforms like FaceTime or Skype, allowing people to receive care safely from home.
- FSA/HSA Flexibility: The CARES Act allowed Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs) to be used for over-the-counter medicines without a prescription. It also made personal protective equipment (PPE) like masks, hand sanitizer, and sanitizing wipes an eligible medical expense. Later legislation also allowed employers to permit employees to carry over all unused FSA funds from 2020 to 2021 and from 2021 to 2022.
For more on these changes, see this resource:
CARES Act Health Plan Provisions.
COBRA and Benefit Plan Deadline Extensions
As mentioned, ARPA's
100% COBRA premium subsidy was a major form of relief from April to September 2021. In addition to that subsidy, the government established an
"Outbreak Period" that paused the clock on many time-sensitive benefit plan deadlines, retroactive to March 1, 2020. This relief extended the time people had to elect COBRA, pay their premiums, file claims for their health plan, and enroll in a group health plan after a qualifying life event like marriage or the birth of a child. This comprehensive approach gave Americans critical breathing room to manage their benefits during a chaotic and overwhelming time. These changes had a major impact on employer-sponsored health insurance. For more information, visit:
More info on Employer Sponsored Health Insurance.
Conclusion
The COVID-19 pandemic was a watershed moment that fundamentally transformed the employee benefits landscape. It exposed deep vulnerabilities in our systems but also spurred incredible innovation and a renewed focus on how we protect and support workers. Policies that once seemed impossible - like 100% COBRA subsidies and federally mandated paid sick leave - became temporary lifelines for millions of Americans and have permanently changed the conversation around what a robust benefits package should include.
The key lesson for both employers and employees is that being proactive about benefits is essential. The pandemic proved that unexpected crises can arise at any time, and understanding your options before you need them is critical for maintaining financial and physical well-being. The legacy of the pandemic is a workforce that now places a much higher value on benefits like comprehensive health coverage, mental health support, paid leave, and flexible work arrangements.

At Kelmeg & Associates, Inc., we've seen how overwhelming it can be to steer health insurance, especially during uncertain times. Whether you're in Lafayette CO, Broomfield CO, Boulder CO, Adams County CO, or anywhere else in Colorado, our team is here to help you make sense of it all.
We provide expert, personalized guidance at no extra cost to you. Whether you need a Medicare plan, individual and family coverage through the marketplace, or the right group health insurance for your business, our goal is to provide clarity and give you peace of mind. The pandemic showed us all that having the right coverage isn't a luxury - it's a necessity.